New York City Chiropractic Physician explains disc bulge vs. disc herniation. What you need to know.
The terms disc herniation, disc bulge are often used interchangeably, but there are real differences and important overlaps. If you have back pain, sciatica, or a recent MRI report, you deserve a clear, practical explanation so you can get the right care. This guide explains the difference, why MRI readings can vary, and what you should do next.
What is the difference between a disc bulge and a disc herniation?
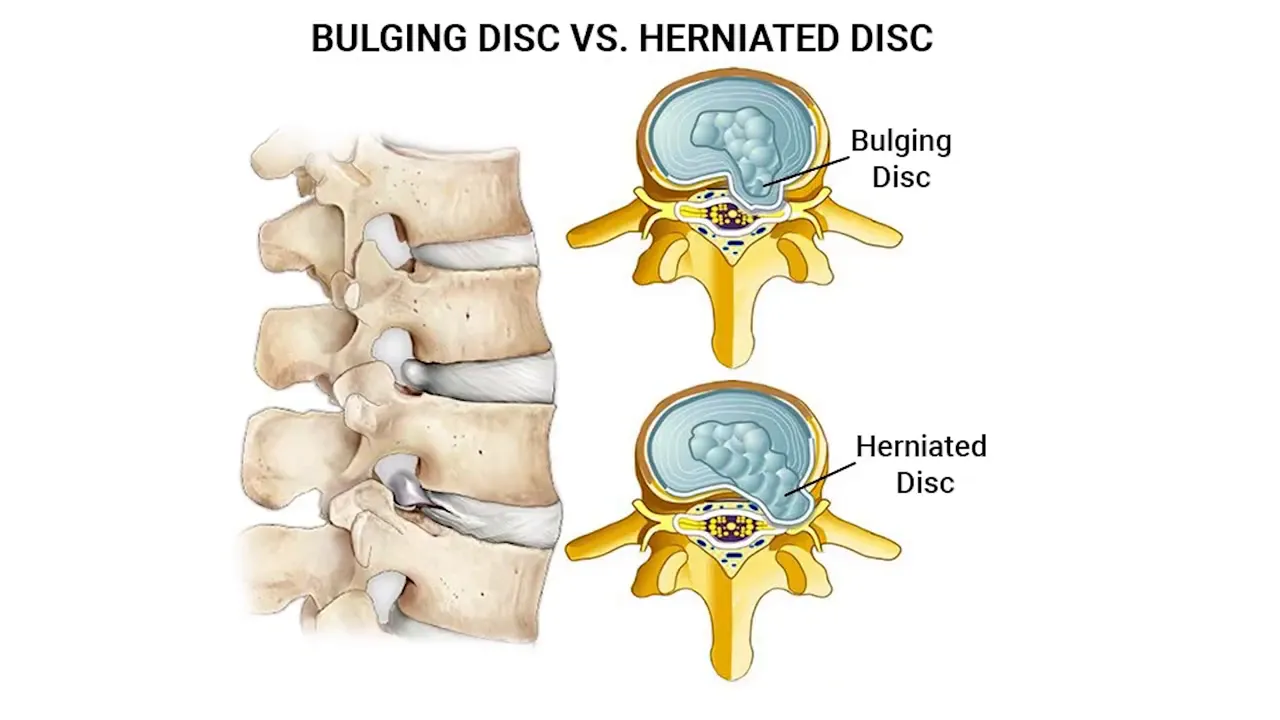
You can think of an intervertebral disc like a jelly donut. The outer layer is tougher and fibrous. A disc bulge happens when the disc material presses outward against that outer fibrous layer but does not break through it. A disc herniation happens when the outer layer is breached and some of the inner material extrudes out, which can press directly on nearby nerves or into the spinal canal.
The distinction is important in anatomical terms: bulge means contained displacement, herniation means a rupture with extrusion. Clinically, however, this distinction does not always change the first steps of care.
Why the bulge versus herniation debate can be confusing
MRI interpretation is subjective
When a radiologist reads an MRI, the final wording of the report can reflect their individual thresholds. One radiologist may call a finding a large disc bulge while another may label the same appearance a small herniation. You might receive two different-sounding reports even though the underlying issue is the same. This variability explains why discussions about bulges and herniations can feel circular and frustrating.
Old herniations can look different
Another wrinkle is time. If a herniation is older, the extruded material may desiccate and shrink. That drying can make it harder to determine whether the outer layer was definitively broken through. In practice, that means an old herniation might appear more like a bulge or disc degeneration (dessication) on imaging even though the rupture occurred earlier.
What this means for your care
Rather than getting hung up on the label, focus on symptoms and functional impact. Whether the report says disc herniation, disc bulge, or something in between, the central point is that you have a disc injury that needs appropriate management.
Your initial plan should center on conservative measures unless there are urgent neurological signs. Typical steps include:
- Targeted physical therapy and guided exercise to restore movement and reduce nerve irritation
- Chiropractic or manual therapy as appropriate to your condition and provider recommendations
- Pain control strategies such as activity modification, short-term medications, and modalities
- Follow-up imaging or specialist referral only if symptoms progress, worsen, or fail to improve
Practical tips when you get an MRI report
- Bring the MRI images with you, not just the report, when you see a specialist.
- Ask your clinician how the imaging findings correlate with your symptoms and physical exam.
- Remember that radiology language can be conservative or aggressive; interpretation should be clinical, not just textual.
- If you are uncertain, a second opinion on imaging is reasonable, especially prior to invasive procedures.
Evidence and perspective
Research shows that imaging findings do not always correlate directly with pain. Many people have asymptomatic disc bulges or small herniations on MRI. That is why your symptoms, neurological exam, and functional limitations guide treatment more than the imaging label alone.
Follow-up with a clinician who evaluates you in person so imaging is integrated into an overall plan that helps you recover and return to the activities you value.
FAQ
How do I know if I have a disc bulge or a disc herniation?
Imaging such as MRI can suggest one or the other, but interpretation is subjective. The best way to know what matters most is an evaluation that links your symptoms and exam findings to the imaging. A provider can explain whether the finding is likely responsible for your pain.
Does a small herniation always require surgery?
No. Many small herniations improve with conservative care including physical therapy, activity modification, and time. Surgery is usually reserved for progressive neurological loss, severe intractable pain, or specific cases where conservative care fails.
Can a disc bulge turn into a herniation?
Yes. A bulge represents outward pressure on the outer layer. With additional stress or degeneration, that outer layer can break down and allow inner material to herniate. That said, not all bulges progress to herniations.
Should I avoid all activity if my MRI shows a disc issue?
No. Absolute rest is rarely the best long-term strategy. Guided, progressive activity and therapy that reduces nerve irritation and restores movement often produce better outcomes than complete inactivity. Always follow your clinician’s individualized guidance.
Final thoughts
You do not need to get stuck on whether a report says disc herniation, disc bulge. What matters is that you address your disc injury with evidence-based care, monitor your symptoms, and work with a clinician who interprets imaging in the context of your exam and goals. With the right approach, many people recover function and reduce pain without invasive measures.
If you are uncertain about your report or your symptoms are worsening, seek evaluation so you can start an appropriate plan and get back to the life you want.
To book a Telehealth visit with an MRI report of findings: SCHEDULE HERE