Blog
 01 Nov 2025
01 Nov 2025
Disc herniation vs. disc bulge: what you need to know
Disc herniation vs. disc bulge: what you need to know.
New York City Chiropractic Physician with over 25 years of experience explains.
The terms disc herniation, disc bulge are often used interchangeably, but there are real differences and important overlaps. If you have back pain, sciatica, or a recent MRI report, you deserve a clear, practical explanation so you can get the right care. This guide explains the difference, why MRI readings can vary, and what you should do next.
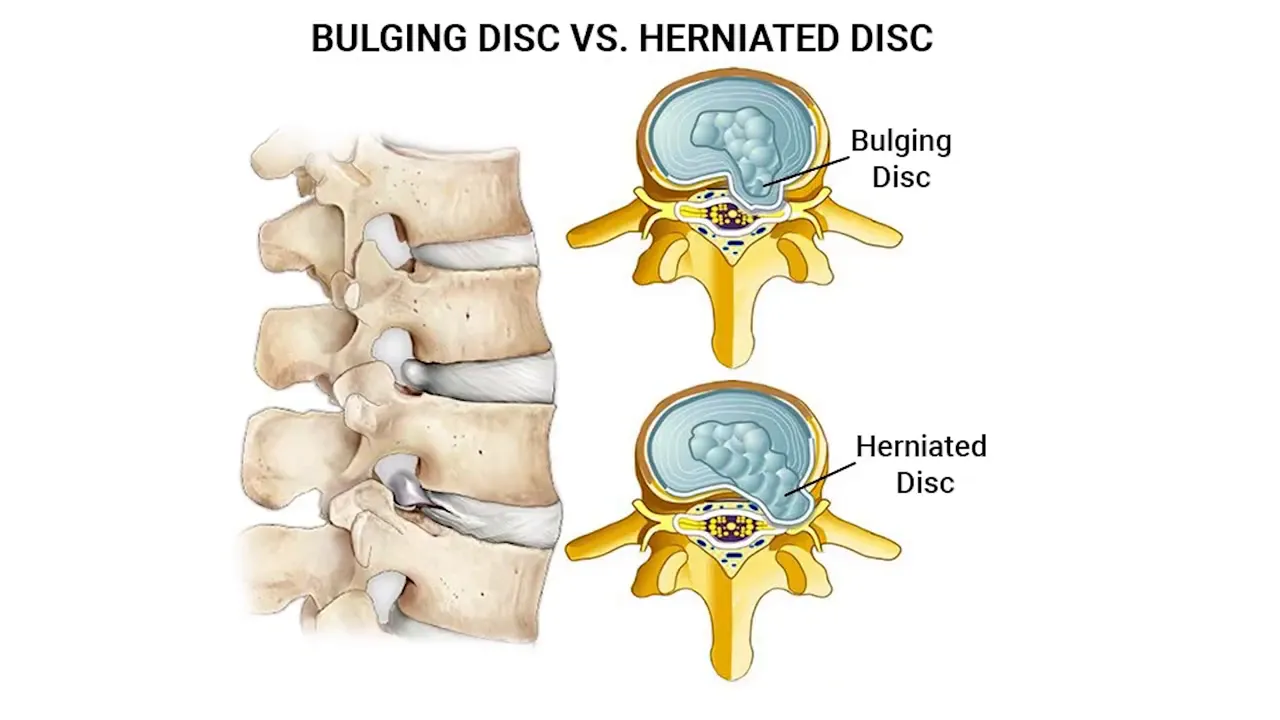
What is the difference between a disc bulge and a disc herniation?
You can think of an intervertebral disc like a jelly donut. The outer layer is tougher and fibrous. A disc bulge happens when the disc material presses outward against that outer fibrous layer but does not break through it. A disc herniation happens when the outer layer is breached and some of the inner material extrudes out, which can press directly on nearby nerves or into the spinal canal.
The distinction is important in anatomical terms: bulge means contained displacement, herniation means a rupture with extrusion. Clinically, however, this distinction does not always change the first steps of care.
Why the bulge versus herniation debate can be confusing
MRI interpretation is subjective
When a radiologist reads an MRI, the final wording of the report can reflect their individual thresholds. One radiologist may call a finding a large disc bulge while another may label the same appearance a small herniation. You might receive two different-sounding reports even though the underlying issue is the same. This variability explains why discussions about bulges and herniations can feel circular and frustrating.
Old herniations can look different
Another wrinkle is time. If a herniation is older, the extruded material may desiccate and shrink. That drying can make it harder to determine whether the outer layer was definitively broken through. In practice, that means an old herniation might appear more like a bulge or disc degeneration (dessication) on imaging even though the rupture occurred earlier.
What this means for your care
Rather than getting hung up on the label, focus on symptoms and functional impact. Whether the report says disc herniation, disc bulge, or something in between, the central point is that you have a disc injury that needs appropriate management.
Your initial plan should center on conservative measures unless there are urgent neurological signs. Typical steps include:
- Targeted physical therapy and guided exercise to restore movement and reduce nerve irritation
- Chiropractic or manual therapy as appropriate to your condition and provider recommendations
- Pain control strategies such as activity modification, short-term medications, and modalities
- Follow-up imaging or specialist referral only if symptoms progress, worsen, or fail to improve
Practical tips when you get an MRI report
- Bring the MRI images with you, not just the report, when you see a specialist.
- Ask your clinician how the imaging findings correlate with your symptoms and physical exam.
- Remember that radiology language can be conservative or aggressive; interpretation should be clinical, not just textual.
- If you are uncertain, a second opinion on imaging is reasonable, especially prior to invasive procedures.
Evidence and perspective
Research shows that imaging findings do not always correlate directly with pain. Many people have asymptomatic disc bulges or small herniations on MRI. That is why your symptoms, neurological exam, and functional limitations guide treatment more than the imaging label alone.
Follow-up with a clinician who evaluates you in person so imaging is integrated into an overall plan that helps you recover and return to the activities you value.
FAQ
How do I know if I have a disc bulge or a disc herniation?
Imaging such as MRI can suggest one or the other, but interpretation is subjective. The best way to know what matters most is an evaluation that links your symptoms and exam findings to the imaging. A provider can explain whether the finding is likely responsible for your pain.
Does a small herniation always require surgery?
No. Many small herniations improve with conservative care including physical therapy, activity modification, and time. Surgery is usually reserved for progressive neurological loss, severe intractable pain, or specific cases where conservative care fails.
Can a disc bulge turn into a herniation?
Yes. A bulge represents outward pressure on the outer layer. With additional stress or degeneration, that outer layer can break down and allow inner material to herniate. That said, not all bulges progress to herniations.
Should I avoid all activity if my MRI shows a disc issue?
No. Absolute rest is rarely the best long-term strategy. Guided, progressive activity and therapy that reduces nerve irritation and restores movement often produce better outcomes than complete inactivity. Always follow your clinician’s individualized guidance.
Final thoughts
You do not need to get stuck on whether a report says disc herniation, disc bulge. What matters is that you address your disc injury with evidence-based care, monitor your symptoms, and work with a clinician who interprets imaging in the context of your exam and goals. With the right approach, many people recover function and reduce pain without invasive measures.
If you are uncertain about your report or your symptoms are worsening, seek evaluation so you can start an appropriate plan and get back to the life you want.
To book a Telehealth visit with an MRI report of findings: SCHEDULE HERE
 19 Oct 2025
19 Oct 2025
Trigeminal Neuralgia Relief: New Treatment Options
Trigeminal Neuralgia Relief
Hi — I’m Dr. David Kulla from Synergy Wellness in New York City. In my video “Trigeminal Neuralgia – NEW Treatment Options,” I explain what trigeminal neuralgia is, discuss common causes, and share a non-drug treatment approach that can provide relief for many people. Below, I walk you through the condition in plain language, explain conventional and emerging techniques, and give clear, practical steps you can try or discuss with your clinician.
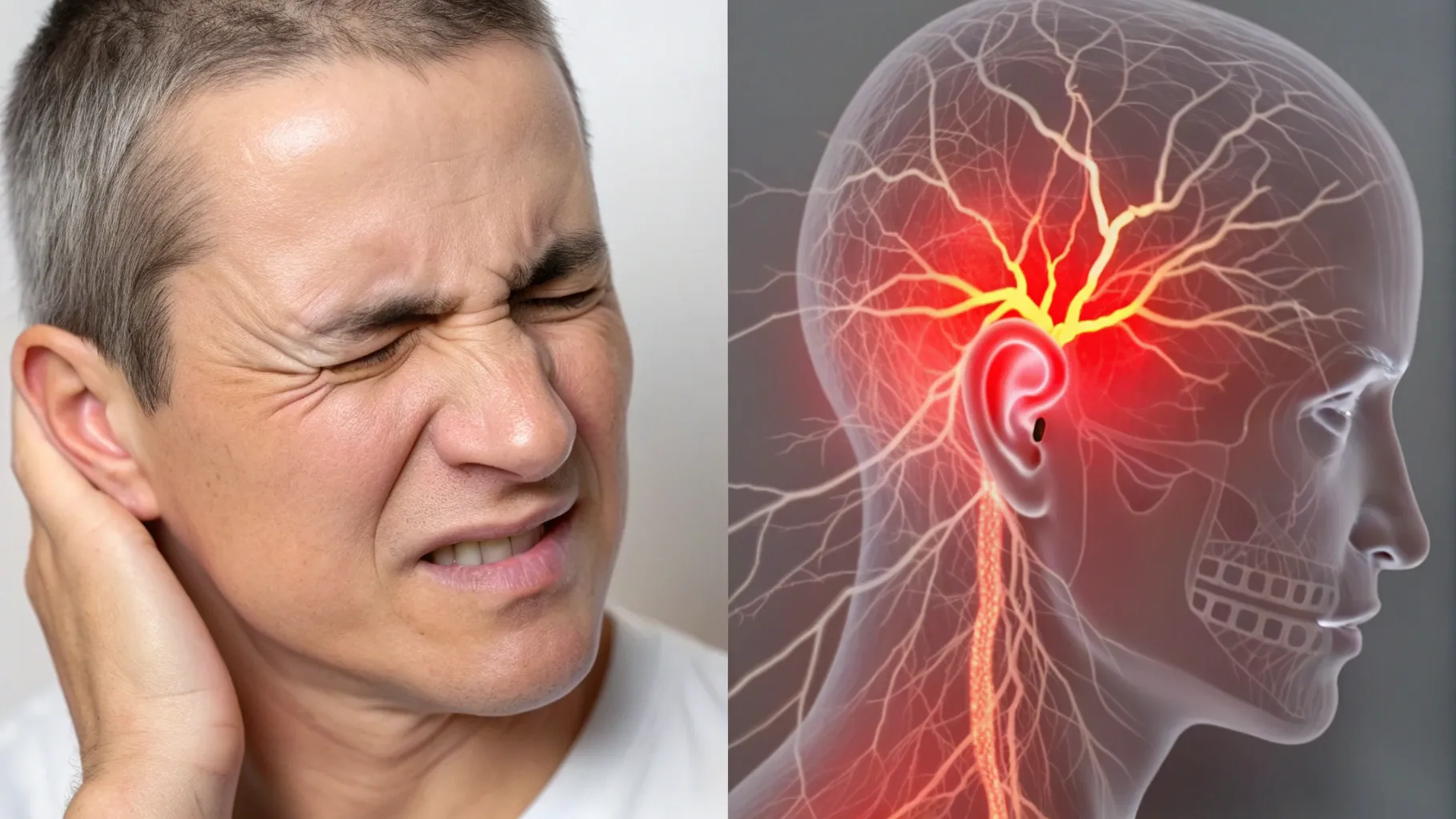
What is trigeminal neuralgia?
Trigeminal neuralgia is a neurological condition that produces sudden, sharp, electric-like pains in the face. It involves irritation of the trigeminal nerve, the major sensory nerve (Cranial Nerve V) for the face. The nerve begins near the ear and splits into three branches: ophthalmic (around the eye and forehead), maxillary (across the cheek), and mandibular (along the jaw). The condition most often affects one side of the face and is more common after age 40.
Common causes and triggers
Several mechanisms can cause or trigger trigeminal neuralgia symptoms:
- Vascular compression: A blood vessel presses on the trigeminal nerve root (vascular compression), producing repeated irritation.
- Jaw and dental factors: Bruxism (teeth grinding), TMJ dysfunction, or jaw misalignment can create muscle tension, spasm, and inflammation that irritate the nerve.
- Trauma: Concussive injuries to the head, neck, or upper back can damage nerve pathways in the brainstem or spinal cord. Symptoms may appear immediately or months to years later.
- Dental procedures: Some people notice the condition after fillings, root canals, or other dental work — sometimes because the nerve pain mimics tooth pain.
How trigeminal neuralgia typically presents
The pain often feels like a quick, stabbing “needle” prick or electric shock pain across the face or cheek or above the eye. It may come on spontaneously or be triggered by light touch, chewing, shaving, or talking. Because the pain can feel intense, many people initially think it’s a tooth problem and seek dental care — sometimes even having teeth removed unnecessarily.
Diagnosis and tests
If you suspect trigeminal neuralgia, a medical evaluation is essential. Your clinician may recommend:
- Neurological exam to check sensory changes and reflexes.
- An MRI is needed to look for vascular compression or other structural causes.
- Referral to a neurologist or neurosurgeon when imaging suggests nerve compression, or a chiropractor equipped with cold laser therapy.
Conventional medical treatments
First-line medical therapy usually involves anticonvulsant medications that reduce nerve firing, in this case the trigeminal nerve, but it targets all nerves. Carbamazepine (brand name Tegretol) is commonly used and can be very effective for many patients. However, medications have side effects and should be reviewed with your prescriber. If you don’t see benefit within a short trial (a few weeks to a couple of months), you and your doctor should reassess.
Cold laser therapy as a non-drug option
At Synergy Wellness, we’ve had success using cold (low-level) laser therapy to reduce inflammation around the trigeminal nerve and provide relief from trigeminal neuralgia. The goal is to calm the irritated trigeminal nerve root and surrounding tissues. Cold laser can be beneficial when symptoms are recent or when patients want to avoid systemic medication side effects.
Practical laser application points
If you have access to a clinical or home cold laser device, the following treatment points cover the trigeminal nerve branches and the nerve root area. (Always follow device instructions and consult a clinician when in doubt.)
- Top or in front of the ear — where the trigeminal nerve wraps above the ear.
- In front of the ear and down along the mandible (jawline).
- On the cheekbone and slightly inward toward the sinus if symptoms involve that region.
- Up at the temple if the ophthalmic branch (around the eye) is painful.
- Behind the ear, pointing upward under the skull toward the brainstem to address the nerve root region.
Some home lasers allow higher-frequency settings (for example, 1,000 Hz). Daily treatments over several days can produce rapid improvement in some people — in our cases, we’ve seen substantial relief within a few sessions when treatments are applied to the correct areas.
Important caution about dental extractions
Because trigeminal neuralgia can mimic tooth pain, people sometimes undergo unnecessary tooth extractions due to the patient’s constant tooth pain. If your dentist says a tooth is healthy, consider trusting that opinion and seeking a neurological evaluation before removing teeth for pain that seems atypical. If needed, get a second dental opinion — but be aware that trigeminal neuralgia can look like dental pain.
When to see a specialist
See a neurologist or neurosurgeon if:
- Your pain is severe, recurrent, or getting worse.
- Imaging suggests vascular compression or another structural cause.
- Medications, chiropractic, and low-level laser therapy are ineffective or intolerable.
Surgical options (microvascular decompression, percutaneous procedures, or radiosurgery) exist for refractory cases and are discussed with patients when conservative measures fail.
Research & further reading
- National Institute of Neurological Disorders and Stroke (NINDS) — Trigeminal Neuralgia: https://www.ninds.nih.gov/health-information/disorders/trigeminal-neuralgia
- Accessible review: Maarbjerg S, Di Stefano G, Bendtsen L, Cruccu G. Trigeminal neuralgia. Lancet Neurol. 2017 — a clinical review (search “Maarbjerg trigeminal neuralgia Lancet Neurol 2017” on PubMed).
- On low-level laser therapy and neuropathic pain: search PubMed for “low-level laser therapy trigeminal neuralgia” to find clinical case reports and small trials describing LLLT use for facial nerve pain.
Conclusion
If you’re reading this because you or someone you care about is dealing with sharp, shock-like facial pain, know that trigeminal neuralgia is treatable. For many people, conservative measures — including careful evaluation, medication trials, and non-drug approaches such as cold laser therapy — can provide meaningful trigeminal neuralgia relief. If you have neck stiffness, headaches, or a history of trauma along with facial pain, mention these to your clinician because they can be important clues. If you have questions about the specific laser approach I use at Synergy Wellness, or to schedule an evaluation, you can contact our office: 212-533-4900 for a consultation.
FAQ
What exactly does trigeminal neuralgia feel like?
It usually feels like a sudden, sharp, electric shock or stabbing pain on one side of the face. Attacks can last for seconds to minutes and may be triggered by touching the face, chewing, speaking, or even a breeze.
Can trigeminal neuralgia be cured?
Some causes, like a blood vessel compressing the nerve, can be addressed surgically (microvascular decompression) and may provide long-term relief. Other patients find effective symptom control with medications or non-drug treatments, including cold laser therapy.
Is cold laser therapy safe, and are there side effects?
Cold (low-level) laser therapy is noninvasive and generally well tolerated, with minimal reported side effects when used properly. Always follow device guidelines and seek clinician guidance for treatment over the skull or near the eyes.
How quickly can I expect trigeminal neuralgia relief with laser therapy?
Response varies. Some patients experience measurable improvement within a few days of daily treatments; others need more sessions. If you don’t improve after a short trial, re-evaluate with your clinician about alternative therapies.
 14 Mar 2025
14 Mar 2025
Chronic Disc Herniations & Spinal Stenosis: Natural Pain Relief
Get Natural Pain Relief Without Surgery in New York City for Chronic Disc Herniations & Spinal Stenosis
Chronic disc herniations, bulges, and spinal stenosis are prevalent spinal conditions that can lead to significant discomfort and impair daily activities and quality of life. Understanding these conditions, their causes, symptoms, and treatment options is crucial for effective management.
 Understanding Disc Herniations and Bulges
Understanding Disc Herniations and Bulges
Intervertebral discs act as cushions between the vertebrae in our spine, comprising a soft, gel-like center encased by a tougher exterior. A disc herniation, often referred to as a slipped or ruptured disc, occurs when the inner nucleus protrudes through a tear in the outer layer, potentially pressing on nearby nerves or causing a chemical irritation to the nerves. This can result in pain, numbness, or weakness in an arm or leg. Interestingly, many individuals with a herniated disc may not experience noticeable symptoms.
What is Spinal Stenosis?
Spinal stenosis involves the narrowing of spaces within the spine, which can exert pressure on the spinal cord and nerves. This condition most commonly affects the lower back and neck, leading to pain, tingling, numbness, and muscle weakness. Over time, these symptoms may progressively worsen.
Common Causes of Disc Herniations and Spinal Stenosis
Several factors contribute to the development of these spinal conditions:
- Aging: Natural wear and tear over time can cause discs to degenerate and lose flexibility, even begin to dehydrate making them more susceptible to herniation or annular tear.
- Degenerative Disc Disease: Discs can break down as you get older, leading to bulging or herniation.
- Arthritis: Osteoarthritis can result in the formation of bone spurs, which may narrow the spinal canal and lead to stenosis.
- Injury: Trauma to the spine can cause immediate disc herniation or accelerate degenerative changes leading to stenosis.
- Scoliosis: Lateral curvature causes premature spinal degeneration.
Associated Symptoms
The symptoms associated with disc herniations and spinal stenosis can vary based on the location and severity of the condition:
- Pain: Localized or radiating pain in the back, neck, arms, or legs.
- Numbness or Tingling: Sensation changes, often in the extremities, due to nerve compression.
- Muscle Weakness: Affected nerves can lead to muscle weakness, impacting mobility and function. Legs can feel heavy, needing to sit often.
- Balance Difficulties: Severe cases may affect coordination and balance.
Conventional Medical Interventions and Their Efficacy
Traditional treatments for these conditions include:
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) and muscle relaxants aim to reduce pain and inflammation. While they can provide temporary relief, they may also cause side effects such as gastrointestinal issues or drowsiness.
- Physical Therapy: Exercises and stretches designed to strengthen the muscles supporting the spine can improve flexibility and reduce pain. Research shows it’s most effective in conjunction with spinal manipulation.
- Surgery: Procedures like discectomy or laminectomy aim to remove or relieve pressure on affected nerves. However, surgical interventions carry risks, including infection, nerve damage, and, in many cases, unfavorable outcomes after 5 years.
Alternative Treatments with Promising Outcomes
Many patients seek non-invasive therapies that offer effective relief with minimal risks. At Synergy Wellness Chiropractic and Physical Therapy in East Village, New York City, we specialize in several such treatments:
- Chiropractic Care: Chiropractic spinal manipulation is recognized for its effectiveness in relieving back, leg, and arm pain.
- Cox Flexion-Distraction Technique: This specialized chiropractic technique gently decompresses the spine, reducing pressure on spinal nerves and discs. It has shown success in treating chronic low back pain, including disc herniations and spinal stenosis, with minimal side effects.
- Cold Laser Therapy: This non-invasive therapy uses low-level laser light to reduce inflammation and promote tissue healing. It offers pain relief with few side effects, making it a great option for those seeking alternatives to medication.
- Spinal Decompression Therapy: This technique involves stretching the spine to relieve pressure on discs and nerves. While some patients may experience mild soreness initially, serious side effects are rare.
Get Relief
Understanding the nuances of spinal conditions and their treatments is essential for effective management. At Synergy Wellness Chiropractic and Physical Therapy, we are committed to providing evidence-based, non-invasive therapies tailored to each patient’s unique needs, aiming to enhance quality of life without the risks associated with more invasive procedures. Synergy Wellness offers a telehealth visit and a second opinion on your MRI or X-rays. Book a Telehealth visit here or call us at (212) 533-4900.
 29 May 2020
29 May 2020
Cold Laser Therapy: treating chronic pain and soft tissue injuries
Cold Laser Therapy for chronic pain and soft tissue injuries

Cold Laser Therapy also known as low level laser therapy is expanding the options for treating chronic pain and soft tissue injuries. Today we are going to talk about everything Cold Laser Therapy. This safe, non-invasive, and effective treatment option opens up a whole new way to treat pain and heal soft tissue injuries caused by many conditions from arthritis to sports injuries and more.
Throughout history, the focus of pain management has largely been on pharmaceuticals. When pain is chronic it becomes a precarious balancing act between maintaining the quality of life and avoiding addictions. The current opioid crisis is a clear indication that innovations in pain treatment are long overdue.
Cold Laser Therapy (LLLT) reduces pain by speeding up your body’s natural healing potential. It’s almost like you’re healing at the speed of light! At Synergy Wellness Chiropractic & Physical Therapy here in New York City, we offer the newest cold laser technology to help you.
Read More “Cold Laser Therapy: treating chronic pain and soft tissue injuries”
 20 May 2020
20 May 2020
Can spinal decompression therapy help with disc bulging and herniation? Yes!
Spinal decompression therapy or traction? Can it help my herniated disc, bulged disc or stenosis?

Spinal decompression therapy can help relieve the pain associated with disc bulging and herniation. In this post, we’re going to get into what spinal decompression is and what it does. We’ll also touch on complementary therapies and other treatment options. Not to be confused with traction which we offer as well.
Traction or decompression, what’s the right fit for you?
For a further explanation on the difference between decompression and traction: WATCH HERE
Why the spine is so important
If you Google the question, “What is the most important part of the body?”, the most common answer is the brain. Because it sends the messages to tell the body what to do it is definitely plays an important role. While that certainly is one of the body’s key organs the spine is the body’s “information highway”. When anything happens to this information delivery system those messages are stuck at home so to speak. The brain and spine make up the nervous system. Combined, they control all of the body’s cells, muscles, tissues, and organs. You only get one spine, and injury and aging cannot be reversed, so you’re definitely going to want to take care of it.
Read More “Can spinal decompression therapy help with disc bulging and herniation? Yes!”
 15 Feb 2020
15 Feb 2020
Treatment for sciatic nerve pain
Treatment of sciatic nerve pain
Treatment for sciatic nerve pain does not have to require invasive procedures or addiction risk. Chiropractic is non-invasive, safe, and effective. In my previous post, Sciatic nerve pain relief, I shared what sciatica is and what causes sciatic nerve pain. Now, let’s compare the available treatments and take a more in-depth look at how and why chiropractic is the best option. Read More “Treatment for sciatic nerve pain”


 Understanding Disc Herniations and Bulges
Understanding Disc Herniations and Bulges